Assisted reproductive technology (ART) refers to all technologies that directly obtain oocytes
from ovaries. The most commonly used technique for fertilization is in vitro fertilization-embryo
transfer (IVF-ET). This process refers to taking out eggs from female ovaries, culturing them in a
vessel containing particular nutrients, and adding a certain amount of technically processed
sperm to fertilize them (IVF phase).
Then the culture is continued, and the early embryo or blastocyst is formed, which is transferred
to the intrauterine implantation (ET phase) to develop into a fetus until delivery. It includes the
second-generation IVF, which is called intracytoplasmic sperm injection (ICSI), the
third-generation IVF, which is called preimplantation embryo genetic screening (PGS) or
diagnosis (PGD).
You may ask how acupuncture connects with IVF and reproductive medicine? As the live birth
rate of assisted reproductive technology is only about 30%-50%, to improve the success rate of
IVF, acupuncture, an ancient therapy, has received attention in the early development of in vitro
fertilization-embryo transfer (IVF) technology.
The world’s first test-tube baby was born in the UK in 1978, but the clinical pregnancy rate was
low. Doctors began to seek help from non-mainstream medicine, meditation, psychological
cues, etc. The application of acupuncture in the field of assisted reproduction also began to
receive attention.
In 1996, Stunner-Victorin et al. published the first research on the application of acupuncture in
IVF and embryo transfer in the “Journal of Human Reproduction,” which ignited acupuncture
points in assisted reproductive technology.
In 2002, Wolfgang E. Paulus applied the evidence-based medicine RCT method for the first
time, using body and ear acupuncture to intervene 25 minutes before and after the IVF embryo
transfer process. As a result, the clinical pregnancy rate can significantly increase, which has
attracted the attention of reproductive endocrinologists.
A live birth determines a successful IVF cycle. The following conditions must be met:
- Quality eggs and sperm;
- Quality diploid embryos;
- Uterine body and endometrial receptivity;
- Embryo development to full term.
So what is the role of acupuncture in reproductive medicine? I conducted a retrospective
analysis of some patients who were successfully treated with acupuncture.
1.Anti-anxiety
There are several situations for those who have high-quality embryos but failed transfers.
Anxiety is one of the most common reasons cause failure. ÎVF procedure is costly, and the
successful way of live birth is only 30%-50%, according to the American Society of Reproductive
Medicine. For some families, children are the bond that maintains the integrity of the family. IVF
becomes their Saviour of marriage or partnership. If IVF is the last straw in the relationship,
tension is understandable.
Anxiety often leads to abnormal secretion of many hormones, such as adrenaline, which can
cause uterine contractions. I have seen a patient who had to terminate the IVF transfer cycle
just three days before the procedure.
However, the uterine contraction never occurred in the subsequent IVF cycle with IVF
acupuncture treatment, and the pregnancy went smoothly. Such patients are good candidates
for IVF acupuncture.
- Reduce uterine artery impedance
If blood flow resistance of the uterine artery increases, the blood supply of the endometrium is
insufficient, affecting the embryo’s implantation and development.
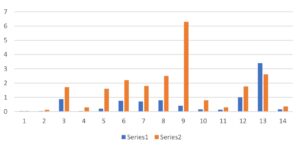
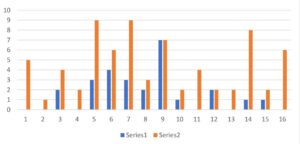
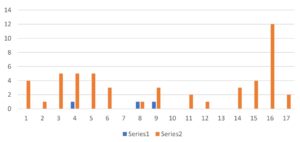
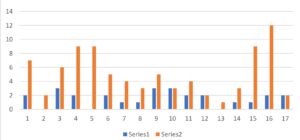
There used to be some reproductive endocrinologists in evidence-based research to observe
patients’ blood flow before and after acupuncture using the uterine artery impedance as an
indicator. I also took part in this observation, and it turned out that the uterine artery impedance
decreased after acupuncture treatment.
- Improving the inflammatory body
Patients with an underlying inflammatory condition, such as immune-endocrine imbalance
levels, unusually elevated estrogen blood levels, imbalance of intestinal microbes, and high
blood viscosity, affect the quality of eggs but also causes intrauterine environment resistance to
implantation.
For mild inflammatory conditions, acupuncture, cupping, and dietary modifications can improve
the body state, making clinical pregnancy possible. Some young patients can also become
pregnant naturally. I have treated a 37-year-old white woman with PCOS. She went through two
failed two egg retrievals. After acupuncture and cupping, the eggs were retrieved, and two
normal blastocysts were obtained. I used to treat a 32-year-old patient with severe arthritis. She
used nearly ten drugs to control the joint pain for a long time. She had failed IUI 6 times. After
acupuncture and dietary modifications for six months, she stopped taking all drugs except 5 mg
dexamethasone and became pregnant naturally. Two years later, she came back for fertility
acupuncture treatment and conceived a second child.
- Adjust the function of the reproductive axis.
Long-term overwork or mental stress may cause adrenal hormones to be often at high levels.
Negative feedback inhibits the secretion of adrenal hormone-releasing hormones, promotes
GnRH release, and damages the reproductive axis. Acupuncture and herbal medicine may help
adjust the neuroendocrine system and restore ovulation to achieve the purpose of natural
pregnancies. There are many successful POI and POF case reports.
- Prevent miscarriage or premature delivery
Contractions caused by various reasons cause many miscarriages or preterm births.
A patient had contractions at the 36th week of pregnancy, and the cervix became shorter in
length. The doctor told her that she would give birth prematurely at any time.
However, after acupuncture treatment, the contractions stopped, and the cervix became stable
and induced labor at forty weeks.